Patient Resources
Get Healthy!
Heart's Electrical Signals Changed in First Pig-to-Human Cardiac Transplant
- October 31, 2022
- Amy Norton HealthDay Reporter
Less than a year after the first-ever transplant of a pig heart into a human patient, doctors are reporting that the heart showed unexpected changes in its electrical system before the recipient ultimately died.
The changes are not believed to have contributed to the patient's death. But experts said that the observation will help in preparing for any such transplants in the future.
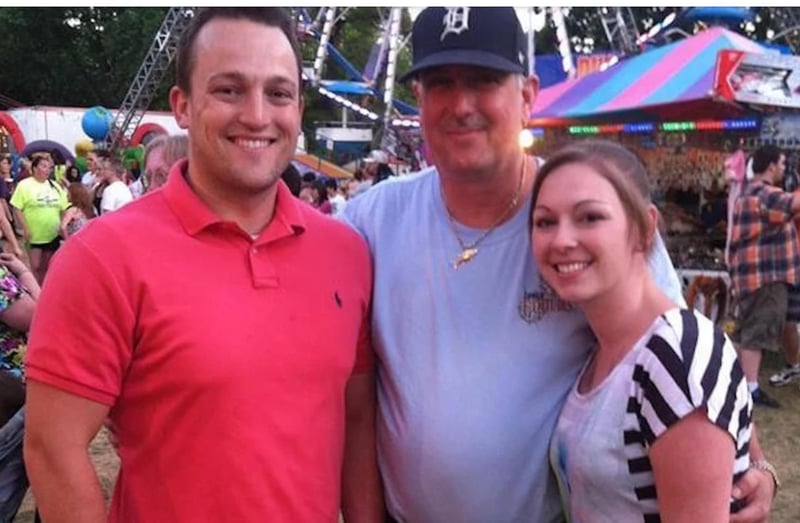
The transplant recipient, 57-year-old David Bennett, died two months after undergoing the groundbreaking procedure last January. The transplant provided him with a pig heart that had been genetically modified to help lessen the chances of his immune system rejecting it.
Bennett had suffered from end-stage heart failure and was out of standard treatment options: He'd been deemed ineligible for a human heart transplant, nor could he receive an implanted mechanical heart pump. Prior to the transplant, he'd been hospitalized for eight weeks with a life-threatening heart arrhythmia.
So his doctors at the University of Maryland Medicine got approval from the U.S. Food and Drug Administration to perform the world's first pig-to-human heart transplant.
The procedure was considered an early success because the heart functioned well, with no obvious signs of rejection, for two months. After Bennett died, his doctors determined that the cause was heart failure -- due to a "complex array of factors." One finding was that the heart contained evidence of a dormant pig virus.
Now the team is reporting that the pig heart also went through some unexpected changes in its conduction system -- the network of cells that transmit the electrical signals that control the heartbeat.
Normally, electrical signals in a pig heart travel very quickly, faster than in a human heart, explained Dr. Timm Dickfeld, a professor at the University of Maryland School of Medicine in Baltimore.
But that was not the case for the transplanted pig heart, he said. Electrocardiogram (ECG) monitoring in the weeks after the procedure showed that electrical signals were traveling far more slowly than would be seen in a pig heart in a pig's body.
Instead, the prolonged travel times were closer to what would be expected in a human heart -- and at times extended beyond what is considered normal. But while that was a concern, there was never a point where doctors had to intervene.
"In Mr. Bennett, we thankfully never saw a need for intervention," Dickfeld said. "We're comfortable saying that we do not believe this contributed to his death."
But, he said, the ECG findings could potentially signal an increased risk of abnormal heart rhythms, and it is something that doctors will need to watch for in any future transplants of this kind.
The findings are scheduled to be presented Saturday at a meeting of the American Heart Association (AHA), in Chicago and online. Studies released at meetings are generally considered preliminary until they are published in a peer-reviewed journal.
The concept of cross-species organ transplants -- called xenotransplantation -- has been under study for years. The hope is to eventually help address the shortage of human donor organs for the seriously ill patients who need them.
In 2021, the U.S. recorded a record number of donor organ transplants, according to the United Network for Organ Sharing. That included more than 3,800 Americans who underwent a heart transplant. However, the demand for donor organs outpaces the supply. As of Oct. 27, 3,368 Americans were on the wait list for a donor heart.
To transplant a pig heart into a human, some major challenges have to be addressed, Dickfeld said: immune system rejection of the organ, infection and the possibility of abnormal heart rhythms.
The pig heart was genetically modified to lessen the chances of immune system rejection, though Bennett still needed immune-suppressing medication. Those genetic modifications are not the reason for the ECG findings, according to Dr. Muhammad Mohiuddin, who directs the university's cardiac xenotransplantation program.
One possible factor, Mohiuddin said, is the solution used to preserve the pig heart after it was harvested. It included hormones such as adrenaline and cortisol, as well as dissolved cocaine.
But figuring out precisely what caused the ECG findings will be tricky and take time, according to Dr. Paul Wang, a professor at Stanford University School of Medicine.
He noted that the transplanted heart was exposed to many factors in the new environment of the human body -- any number of which might have contributed to the changes in the conduction system.
On top of that, Wang said, it's not possible to compare Bennett's case with any prior experience. It's unclear whether the ECG changes were unique to him, or part of the process of transplanting a pig heart into a human, or could ultimately put any future transplant recipients at heightened risk of arrhythmias.
"One can't really say whether these ECG findings were 'bad' or 'good,'" said Wang, who is also editor-in-chief of the AHA journal Circulation: Arrhythmia and Electrophysiology. "This is a phenomenon that was observed."
Wang called the procedure a "true milestone," and said the ECG observations will be useful in moving forward with cardiac xenotransplantation.
More information
The United Network for Organ Sharing has more on heart transplantation.
SOURCES: Timm Dickfeld, MD, PhD, professor, medicine, and director, electrophysiology research, University of Maryland School of Medicine, Baltimore; Muhammad Mohiuddin, MBBS, professor, surgery, and scientific/program director, cardiac xenotransplantation program, University of Maryland School of Medicine; Paul Wang, MD, professor, medicine and bioengineering, Stanford University School of Medicine, and director, Stanford Cardiac Arrhythmia Service, Stanford, Calif.; presentation, American Heart Association annual meeting, Nov. 5, 2022, Chicago and online

